The Benefits of AI for Medical Radiological Diagnosis, What is the Accuracy and What are the Issues Behind it?
Jakarta, 11 August 2023 - Radiology has undergone a major transformation thanks to artificial intelligence (AI) in medical diagnosis.
In recent years, AI has brought revolutionary changes, including in the field of radiology.
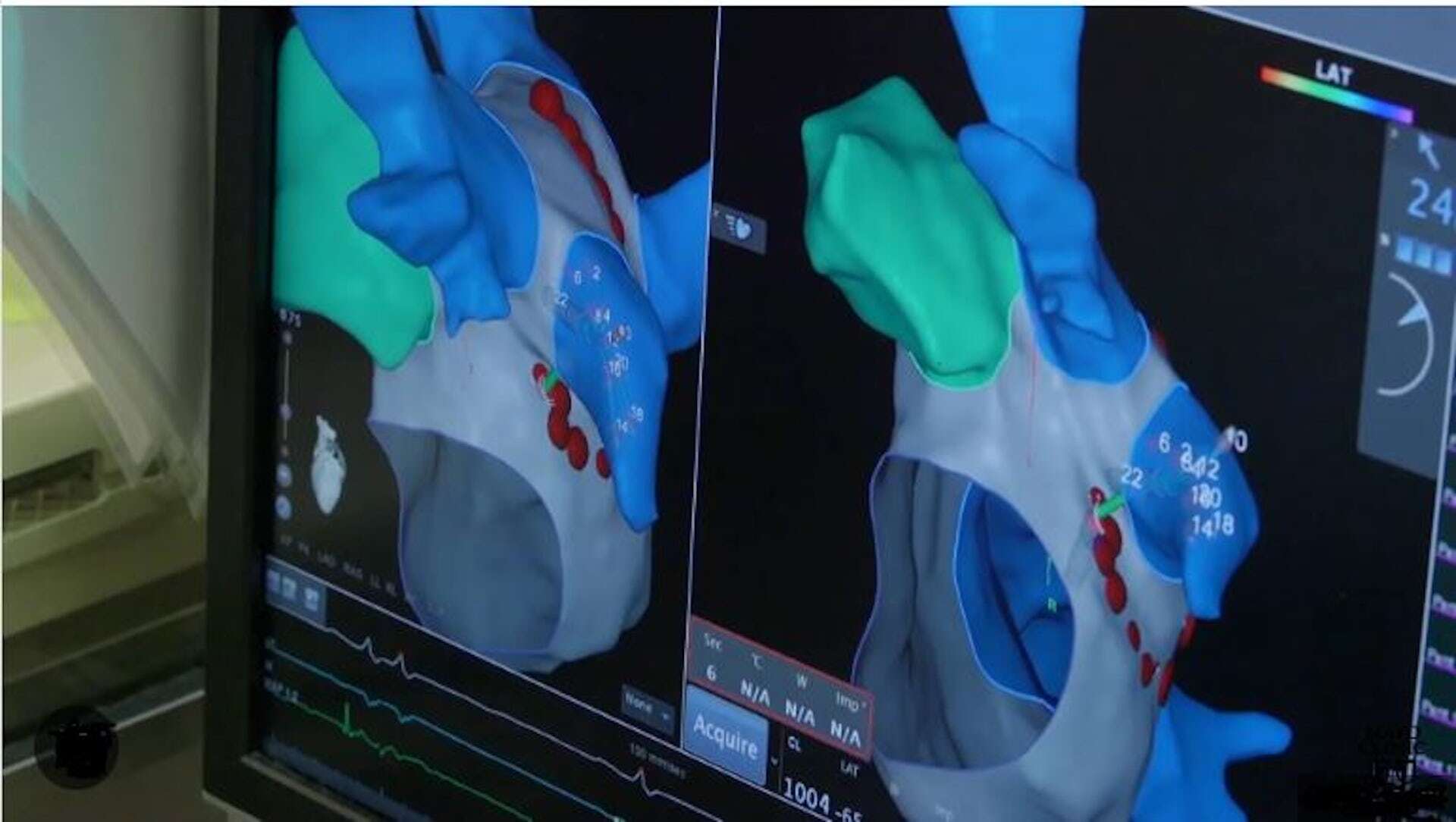
Through the use of AI techniques such as machine learning to recognise medical image patterns, deep learning to analyse medical images with high accuracy, and computer vision to examine visual images, radiology has undergone a fundamental change in the way it interprets medical images and diagnoses diseases.
Radiology is a medical discipline that uses medical images to diagnose diseases and treat them. Radiology technology produces medical images through sound waves (ultrasound/USG), X-rays (X-rays, CT scans) and magnetic fields (MRI) to detect, visualise and diagnose various medical conditions.
However, conventional radiology still faces challenges in interpreting medical images with high efficiency and accuracy. This process requires a long time and high expertise from the radiologist. Interpretation errors can negatively impact patient care.
In this context, AI emerges as a promising solution due to its high speed and accuracy. In radiological diagnosis of hip fracture cases, for example, a UK study showed that radiologists only diagnosed 77.5% of images accurately, while AI machine learning systems were able to achieve 92% accuracy.
From this research report, there is a 14.5% chance that patients who are not diagnosed by radiologists will receive inadequate or inappropriate therapy and treatment because they are not properly diagnosed.
However, several studies have shown a lack of AI-related knowledge in hospital radiology departments.
Benefits of radiological diagnosis
Accurate and prompt radiological medical diagnosis is essential in disease management and patient care. There are many diseases that require radiological diagnosis both non-communicable and communicable diseases.
For example, detecting cancer or tumours. All organ sites (such as lungs, breasts, colon) suspected of having cancer cells or tumours can be diagnosed using radiological imaging techniques such as CT scans, MRIs, and positron emission tomography (PET) scans.
Radiological diagnosis is also used to determine the location and type of fracture. This will determine the type of treatment and subsequent therapy. CT scans can assess head injuries, such as brain haemorrhage or skull fractures. Cardiac CT scan and coronary angiography to detect and evaluate heart conditions such as narrowed coronary arteries.
Detecting problems around the abdomen, such as gallstones, kidney stones, infected appendix, hernia, also requires a CT scan. Inflammation of the joints, such as the knee or hip, also requires radiological diagnosis to assess the extent of joint damage.
In the context of infectious diseases, radiological diagnosis is performed for cough complaints suspected to be related to lung diseases such as infections (pneumonia, tuberculosis).
In these cases, early radiological detection is essential to detect any changes or abnormalities in organs or tissues early.
Proper management and treatment can be carried out immediately so that patients can increase their chances of recovery or reduce (prevent) the risk of more serious complications. A proper diagnosis also helps the medical team in planning the treatment that suits the patient's needs.
Information from radiological diagnosis also plays an important role in clinical decision-making, such as treatment options, surgical decisions, or follow-up measures.
Interdisciplinary collaboration, supported by accurate radiological diagnosis, can facilitate communication between medical specialists and enable holistic patient care. Interdisciplinary collaborations include radiology, pathology (cell and tissue specialists), clinical lab, cardiology (cardiologists), nephrology (kidney specialists), gastroenterology (gastroenterologists), oncology (tumour specialists), psychiatry and immunology (immune specialists).
In addition to the above disciplines, there are many other clinical specialists such as pulmonologists, allergists, rheumatologists, surgeons, who are involved in interdisciplinary cooperation for a comprehensive and integrated medical diagnosis.
AI is promising but has many challenges
AI can recognise patterns that may be difficult for humans to detect, enabling early identification of diseases and providing more precise treatment recommendations.
A literature research shows that the use of AI produces an average accuracy of over 80% to analyse and detect CT scans of the lungs of people infected with COVID-19 quickly.
Although promising, there is no open data showing the application of AI in radiology in hospitals and medical laboratories in Indonesia. The use of AI for non-radiology, such as for telemedicine applications has started at Universitas Indonesia Hospital in Depok.
Other countries are also active in adopting AI technology in radiology. Some countries have strengthened the use of AI in radiology through specific policies and regulations that support the development and application of this technology.
Several countries such as the United States, United Kingdom, Germany, and Singapore have guidelines and standards for the validation and use of AI in radiology to ensure safety and accuracy in its application.
While Indonesia does not yet have AI-related regulations, it is important to note that regulations and guidelines are constantly being updated and evolving along with the development of AI and medical technology as a whole.
In the process of transforming radiology with AI, conventional radiology faces several challenges. Some of the common challenges include lack of quality data, integration with existing radiology systems, meaningful interpretation, data privacy and security, integration in radiology workflows, and trust and adoption of technology and work systems.
Although radiology transformation with AI offers many benefits, it is important to understand that AI is not a substitute, but a tool for radiologists.
Radiologists continue to have an important role in patient interpretation and management. With deep clinical expertise and the ability to integrate clinical information, radiologists are key actors in decision making.
AI can assist in some radiology tasks, but human excellence in comprehensive evaluation and understanding of patient context remains irreplaceable.